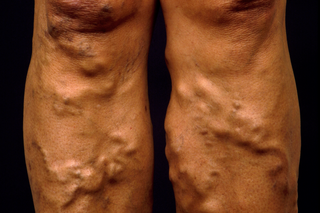
Check if you have varicose veins
Varicose veins are widened veins that look swollen and twisted under the skin. They may feel lumpy and bulge out.
They're most common on the legs, but you can get them on other parts of your body.

They sometimes cause other symptoms that affect your legs, such as:
- pain, aching or a feeling of heaviness
- skin changes, such as itching, colour changes or dry, scaly skin
- swollen ankles or legs
The symptoms may be worse after standing for a long time, and may get better when you rest with your legs up.
Varicose veins may get worse without treatment, but this usually happens very slowly over several years.
They are different from spider veins or thread veins – small red, blue or purple veins that are usually harmless.
Things you can do to help with varicose veins
If you have varicose veins, there are things you can do to help with the symptoms.
Do
-
try to keep to a healthy weight
-
put your legs up when possible – for example, lie down with your legs on cushions
-
exercise regularly, such as running or walking, to improve blood flow
-
use a moisturising cream or lotion if you have dry, flaky or itchy skin
-
try not to injure your legs, to help prevent bleeding
Don’t
-
do not stand for long periods
-
do not sit for long periods, unless your feet are raised
-
do not smoke, as it damages your veins – get help to quit smoking
Non-urgent advice: See a GP if:
You have varicose veins and:
- you have symptoms such as pain, itching or swelling in your legs
- you get a sore on your leg that has not healed after 2 weeks
Urgent advice: Ask for an urgent GP appointment or get help from NHS 111 if:
- you have varicose veins that are bleeding
You can call 111 or get help from 111 online.
Treatment for varicose veins
Varicose veins do not always need treatment. A GP may refer you to a specialist for tests and treatment if you have:
- symptoms such as pain, heaviness, swollen legs, itching or skin changes
- any complications, such as ulcers on your legs
Treatment to improve how varicose veins look is not usually available on the NHS if they're not causing any other problems. You may be able to pay for it privately.
Assessment and treatment from a specialist
If you're referred to a specialist they'll usually do a test called duplex ultrasound to confirm if you have varicose veins and plan your treatment. This is a type of scan to check your blood flow.
There are several types of treatment that may be offered, including:
- procedures to block blood flow in the veins, such as endothermal ablation and foam sclerotherapy
- surgery to remove varicose veins
- compression stockings
The specialist will explain which treatment may be best for you, and the benefits and risks.
Treating varicose veins in pregnancy
If you get varicose veins during pregnancy, you may be able to use compression stockings, but procedures or surgery to treat them are not usually recommended while you're pregnant.
Varicose veins often get better or go away after your baby's born.
Causes of varicose veins
Varicose veins happen when the valves that control the flow of blood in your vein do not work properly. This causes blood to build up and put pressure on the vein, which makes it swell and twist.
Varicose veins are very common and anyone can get them, but it's more likely to happen if you:
- are a woman
- are older
- are overweight
- are pregnant
- spend a lot of time standing or sitting
- have other family members with varicose veins
- have had deep vein thrombosis (DVT)
Complications of varicose veins
Varicose veins do not usually cause any serious problems. But they can sometimes cause complications including:
- bleeding
- itchy, flaky, dry skin over your veins (varicose eczema)
- sores that take a long time to heal (venous leg ulcers)
- blood clots under your skin that cause hard, painful veins (superficial vein thrombosis)
- blood clots deeper inside your leg (deep vein thrombosis – DVT)
Page last reviewed: 01 July 2024
Next review due: 01 July 2027